The healthcare industry is no stranger to complex billing practices and regulatory requirements, but when providers engage in fraudulent activities, taxpayers pay the price.
In a recent case, a chronic disease management healthcare provider, Bluestone Physician Services, has been held accountable for submitting false claims to the Florida Medicaid program, resulting in a substantial financial settlement.
Bluestone Physician Services, along with its affiliated entities, Bluestone Physician Services of Florida, LLC, and Bluestone National, LLC, were accused of violating the federal False Claims Act and the False Claims Acts of Florida and Minnesota.
Read: Combating Odometer Fraud: AG Ashley Moody’s Crusade To Protect Florida Consumers
The allegations centered around the provider’s submission of false or fraudulent claims for certain evaluation and management codes related to services provided to chronic care patients in assisted living and other care facilities.
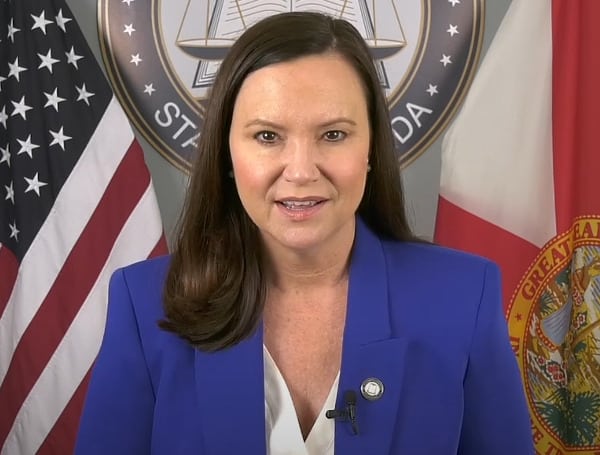
The investigation into Bluestone’s billing practices was the result of a whistleblower lawsuit filed in the United States District Court for the Middle District of Florida. Florida’s Attorney General Ashley Moody’s Medicaid Fraud Control Unit (MFCU) collaborated with their counterparts in Minnesota and the federal government to uncover the extent of the fraudulent activity.
“This chronic disease management health care provider sought payments from Medicare and Medicaid for higher, more expensive levels of medical services than those actually performed and payments for medically unnecessary services. This type of activity results in the overpayment of taxpayer funds through these programs. Thanks to the hard work of our Medicaid Fraud Control Unit, we have secured a nearly $600,000 payment to Florida Medicaid for these fraudulent claims,” said Florida Attorney General Ashley Moody.
Read: Four Men Now Charged In Florida Carjacking, Kidnapping That Left 31-Year-Old Woman Dead
As a result of the multistate action, Bluestone Physician Services, Bluestone Physician Services of Florida, LLC, and Bluestone National, LLC agreed to pay millions of dollars in settlement fees. Florida Medicaid, in particular, will receive a substantial $593,038 payment, which represents a significant recovery of taxpayer funds that were wrongfully obtained.
The Florida Attorney General’s Medicaid Fraud Control Unit (MFCU) played a crucial role in this case, investigating and prosecuting the provider’s fraudulent billing practices. The MFCU is responsible for safeguarding the state’s Medicaid program by identifying and addressing fraud, abuse, and exploitation.
The Florida MFCU is funded through a grant from the U.S. Department of Health and Human Services Office of Inspector General. The federal government provides 75% of the funding, and the state of Florida contributes the remaining 25%. This collaborative funding model ensures that the MFCU has the necessary resources to carry out its vital mission.
Help support the Tampa Free Press by making any small donation by clicking here.
Android Users, Click To Download The Tampa Free Press App And Never Miss A Story. Follow Us On Facebook and Twitter. Sign up for our free newsletter.