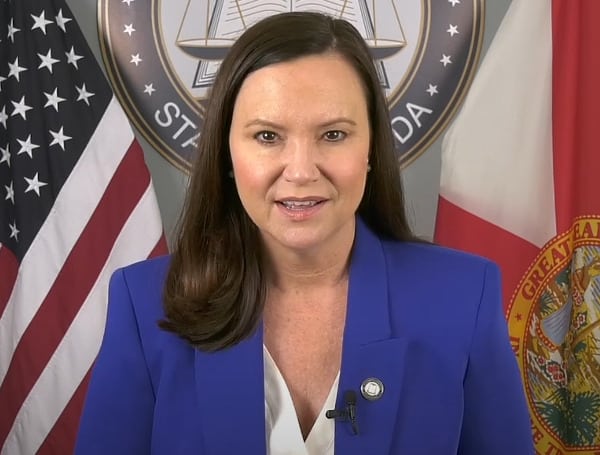
In collaboration with federal and state authorities, Florida Attorney General Ashley Moody’s Medicaid Fraud Control Unit has recovered over half a million dollars for Florida Medicaid from laboratory service providers accused of fraudulent billing practices.
Attorney General Ashley Moody said, “Our Medicaid Fraud Control Unit has recovered more than half a million dollars for Florida Medicaid from several medical companies that manipulated claims and attempted to game the system by adding diagnosis codes to claims submitted to Medicare and Medicaid, which were not provided by the beneficiaries’ physicians. We will continue working to stop those defrauding these taxpayer-funded programs.”
Read: Federal Judge Allows Challenge To Florida Teacher Pronoun Law To Proceed
The companies Vista Clinical Diagnostics, LLC, Access Dermpath, Inc., and Advanced Clinical Laboratories, Inc. allegedly violated the False Claims Act by submitting false or inflated laboratory testing claims to Medicaid and Medicare. The companies reportedly manipulated diagnosis codes on claims without the knowledge or authorization of the patient’s physicians.
The settlement agreement resolves allegations that the companies manipulated diagnosis codes manually and electronically, inserting codes not provided by the referring physician into their reimbursement claims.
This action stemmed from a whistleblower lawsuit filed in the United States District Court for the Middle District of Florida. Vista Clinical Diagnostics subsequently filed for bankruptcy, and the settlement agreement was approved by the United States Bankruptcy Court on July 9.
Help support the Tampa Free Press by making any small donation by clicking here.
Android Users, Click To Download The Tampa Free Press App And Never Miss A Story. Follow Us On Facebook and Twitter. Sign up for our free newsletter.